If you are a head or assistant coach or manager, and you have not taken a concussion training in the last three years, as required by the State of Michigan, please do so and provide a copy of your concussion certificate via email to office@kvhockey.org.
If you are a head or assistant coach or manager, and you have not taken a concussion training in the last three years, as required by the State of Michigan, please do so and provide a copy of your concussion certificate via email to office@kvhockey.org.
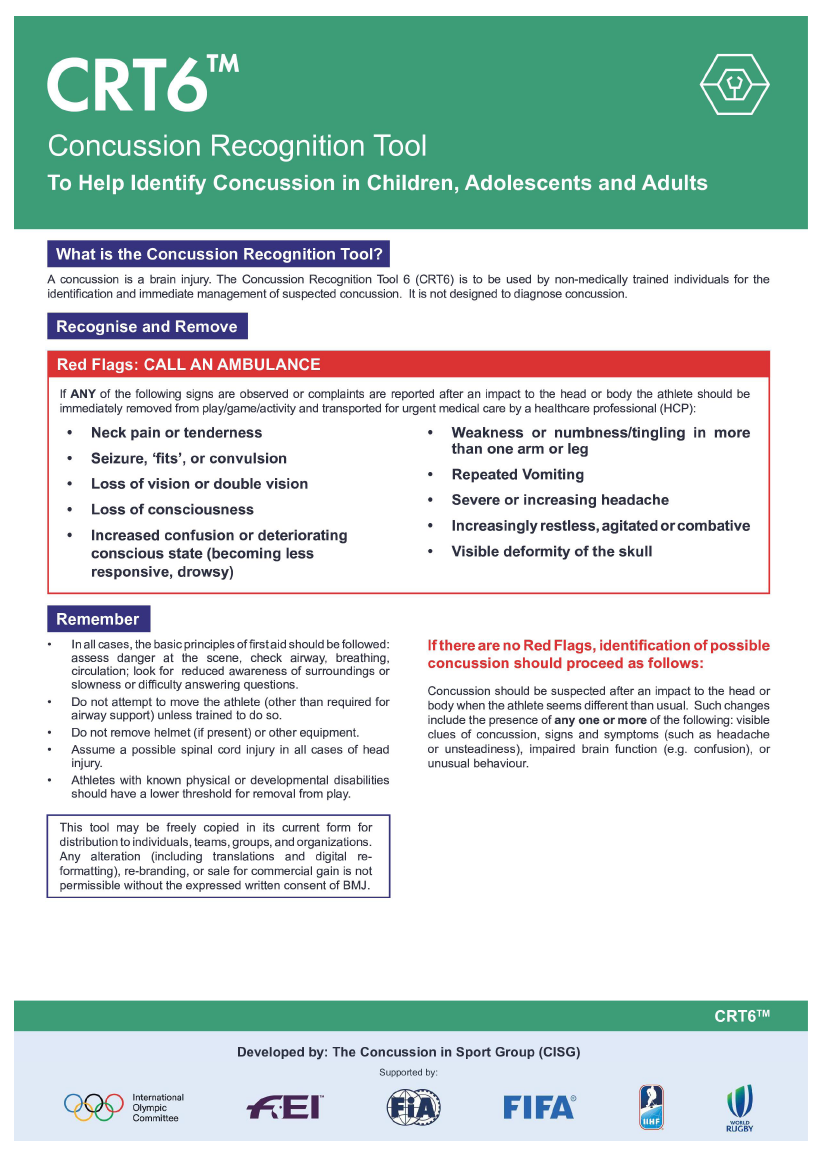
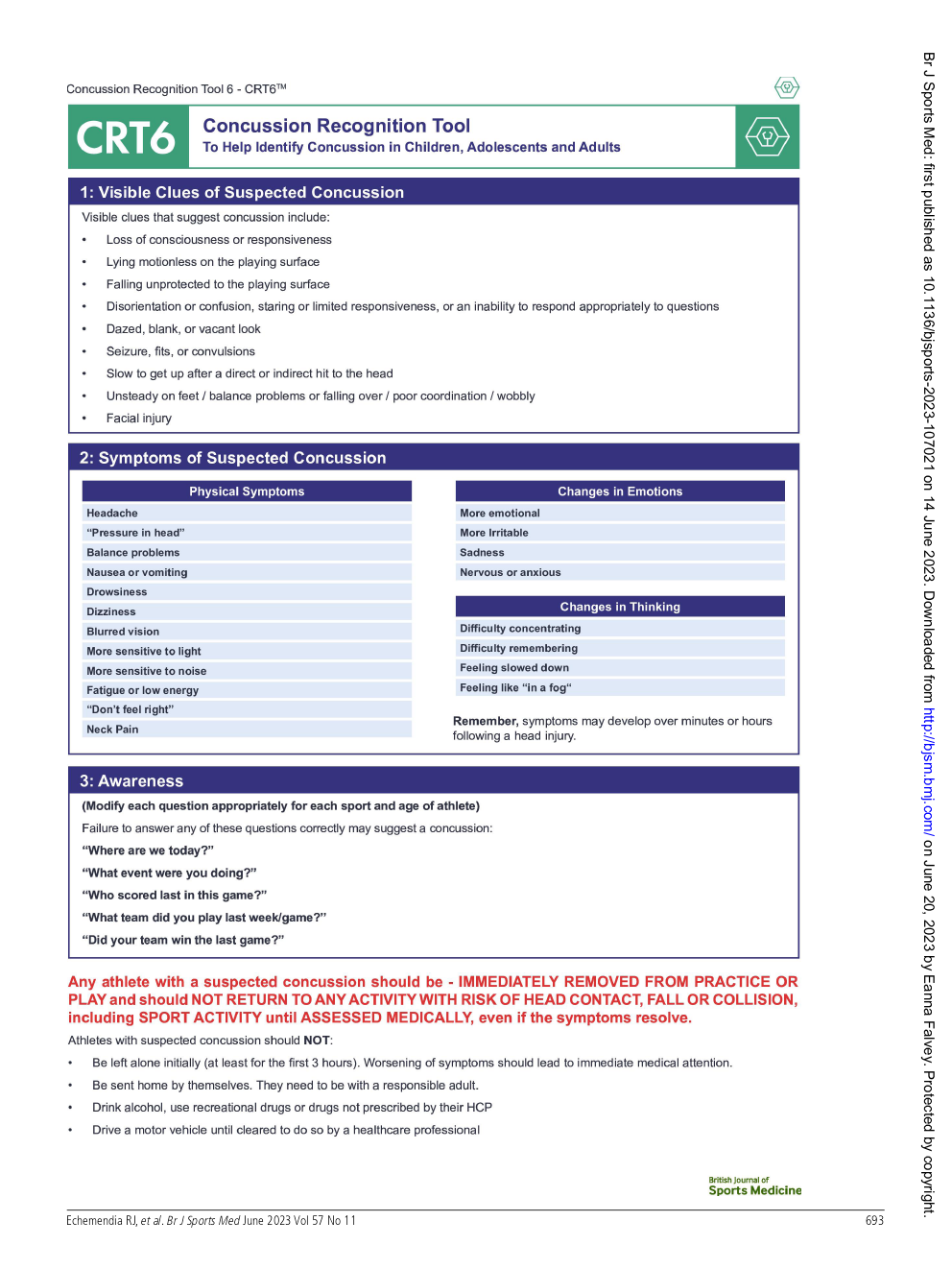
A player who experiences an impact from an open-ice check, an unanticipated or incidental hit, collision or blows to the head or neck, or by a fall or contact with the boards should be immediately assessed by a coach on the bench for a possible concussion. Coaches should familiarize themselves with the CTR6 -Concussion Recognition Tool, and visually assess the player's actions and behavior, ask the player questions, what rink they are on, what day is it, mom or dads name, when is their birthday, stuff they would know. Additionally, ask the player how they are feeling. If a player appears to be unable to skate that is a SIGN of a concussion, if he/she reports that she is too dizzy to skate that is a SYMPTOM of a concussion. Either one would require sitting out and a clinical evaluation by a medical professional by initiating the following concussion protocol:
3. Inform the player’s parents or guardians that returning to play requires an assessment by a medical professional
4. Initial assessment and treatment typically includes a period of rest of uncertain length to be determined by the medical professional until symptoms and signs resolve.
5. Begin a graded return-to-learn/school and then sport.
6. Provide written medical clearance from the medical professional for return to play utilizing the USA Hockey Return to Play Form (required).
USA Hockey’s Concussion Management Program can be found below and on the USA Hockey website at: usahockey.com/safety-concussion
 2023 USA Hockey Concussion Management Program
2023 USA Hockey Concussion Management Program
Michael Stuart, MD; Kevin Margarucci, ATC
A sports concussion management program must be incorporated within each affiliate. All USA Hockey programs should follow this protocol as a minimum standard and conform to their individual state concussion statutes.
Accepted current medical practice and the law in most states requires that any athlete with a suspected Sports Related Concussion (SRC) is immediately removed from play.
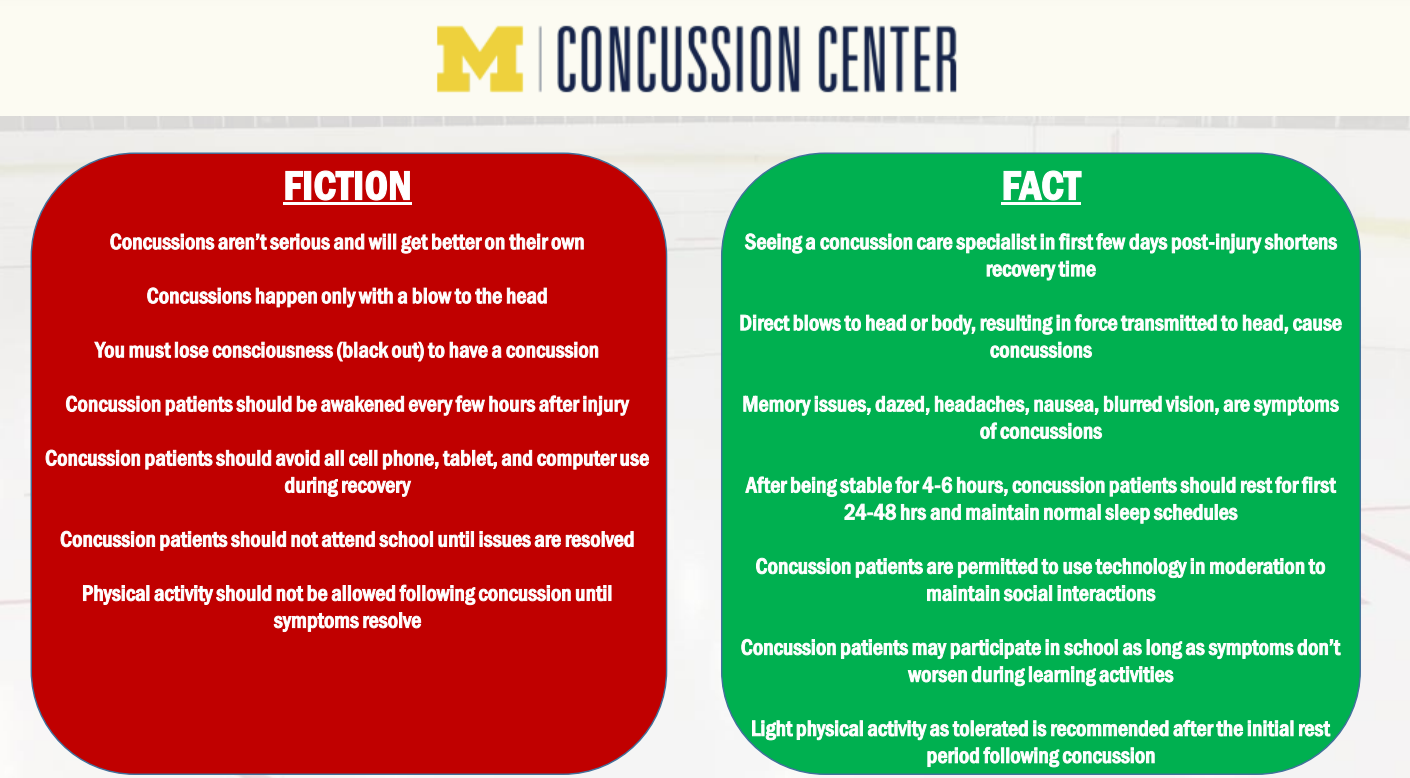
• A concussion is a traumatic brain injury- there is no such thing as a minor brain injury.
• A player does not have to be “knocked-out” to have a concussion- less than 10% of players lose consciousness.
• A concussion can result from a blow to head, neck, or body.
• Concussions often occur to players who don’t have or just released the puck, from open-ice hits, unanticipated hits, and illegal collisions.
• The youth hockey player’s brain is more susceptible to concussion.
• Concussion in a young athlete may be harder to diagnosis, takes longer to recover, and is more likely to have a recurrence, which can be associated with serious long-term effects.
• The strongest predictor of slower recovery from a concussion is the severity of initial symptoms in the first day or 2 after the injury.
• Treatment is individualized and it is impossible to predict when the athlete will be allowed to return to play- there is no standard timetable.
A player with any symptoms/signs or a worrisome mechanism of injury has a concussion until proven otherwise:
“When in doubt, sit them out.”
Follow these concussion management steps:
1. Remove immediately from play (training, practice, or game)
2. Inform the player’s coach/parents or guardians.
3. Refer the athlete to a qualified health-care professional (as defined in state statute)
4. Initial treatment requires a short period of rest, but the athlete may participate in light exercise (if their symptoms are not made worse).
5. Begin a graded return-to-sport and return-to-learn.
6. Provide written medical clearance for return to play (the USA Hockey Return to Play Form is required)
Diagnosis
Players, coaches, officials, parents, and heath care providers should be able to recognize the symptoms/signs of a sport related concussion. (See attached Concussion Recognition Tool 6)
Symptoms:
• Headache
• “Pressure in head”
• Neck Pain
• Nausea or vomiting
• Balance problems
• Dizziness
• Drowsiness
• Blurred vision
• Difficulty concentrating/remembering
• “Don’t feel right”
• Sensitivity to light/noise
• More emotional or irritable
• Fatigue or low energy
• Feeling like “in a fog”
• Feeling slowed down
• Confusion
• Sadness
• Nervous or anxious
Observable Signs:
• Lying motionless on the playing surface
• Slow to get up after a direct or indirect hit to the head
• Disorientation or confusion
• Inability or slow to respond appropriately to questions
• Blank or vacant look
• Slow movement or incoordination
• Balance or walking difficulty
• Facial injury after head trauma
Management Protocol
1. If the player is unresponsive- call for help & dial 911
2. If the athlete is not breathing: start CPR
3. Assume a neck injury until proven otherwise
✓ DO NOT move the athlete.
✓ DO NOT rush the evaluation.
✓ DO NOT have the athlete sit up or skate off until you have determined:
• no neck pain
• no pain, numbness, or tingling
• no midline neck tenderness
• normal muscle strength
• normal sensation to light touch
4. If the athlete is conscious & responsive without symptoms or signs of a neck injury…
• help the player off the ice to the locker room.
• perform an evaluation.
• do not leave them alone.
5. Evaluate the player in the locker room: Concussion Recognition Tool 6 or other sideline assessment tools
• Ask about concussion symptoms.
• Observe for concussion signs.
• Memory Assessment
→ What venue are we at today?
→ What period is it?
→ Who scored last in this game?
→ Did your team win the last game?
→ Who was your opponent in the last game?
→ If a healthcare provider is not available, the player should be safely removed from practice or play and referral to a physician arranged.
6. A player with any symptoms or signs, disorientation, impaired memory, concentration, balance, or recall has a concussion and should not be allowed to return to play on the day of injury.
7. The player should not be left alone after the injury, and serial monitoring for deterioration is essential over the initial few hours after injury
If any of the signs or symptoms listed below develop or worsen go to the hospital emergency department or dial 911.
➢ Severe throbbing headache
➢ Dizziness or loss of coordination
➢ Ringing in the ears (tinnitus)
➢ Blurred or double vision
➢ Unequal pupil size
➢ No pupil reaction to light
➢ Nausea and/or vomiting
➢ Slurred speech
➢ Convulsions or tremors
➢ Sleepiness or grogginess
➢ Clear fluid running from the nose and/or ears
➢ Numbness or paralysis (partial or complete)
➢ Difficulty in being aroused
8. Concussion symptoms & signs evolve over time- the severity of the injury and estimated time to return to play are unpredictable.
9. A qualified health care provider guides the athlete through Return-to-Learn and Return-to-Sport strategies.
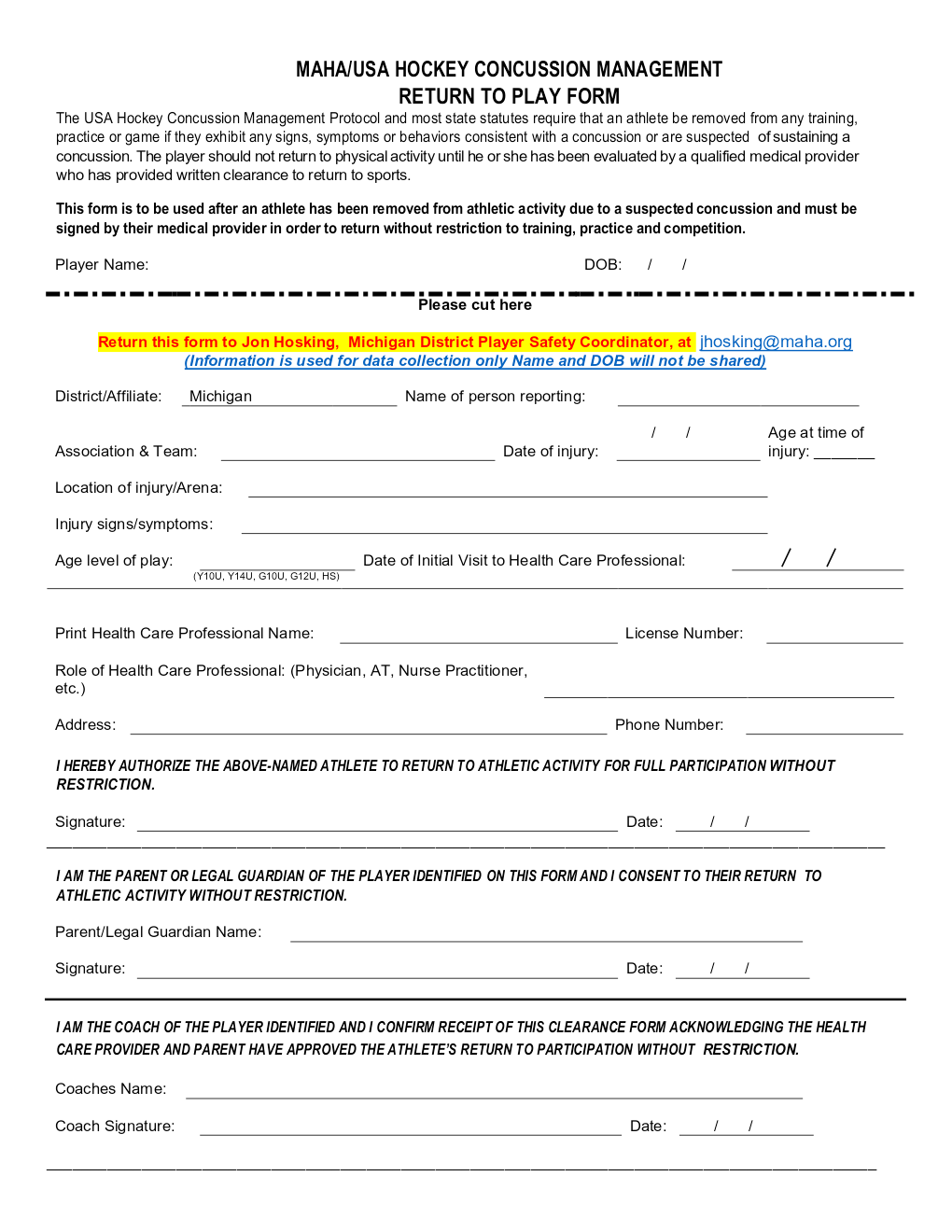
10. Written clearance from a qualified health care provider is required for an athlete to return to play without restriction (training, practice, and competition). Only the USA Hockey Return to Play Form is acceptable:
MAHA Concussion Management - https://www.maha.org/concussions
USA Hockey Concussion Management Program - https://www.usahockey.com/safety-concussions
USA Hockey Concussion Management Return to Play Form - https://cdn1.sportngin.com/attachments/document/0057/6528/USA_Hockey_Concussion_Management_Return-to-Play_Form.pdf
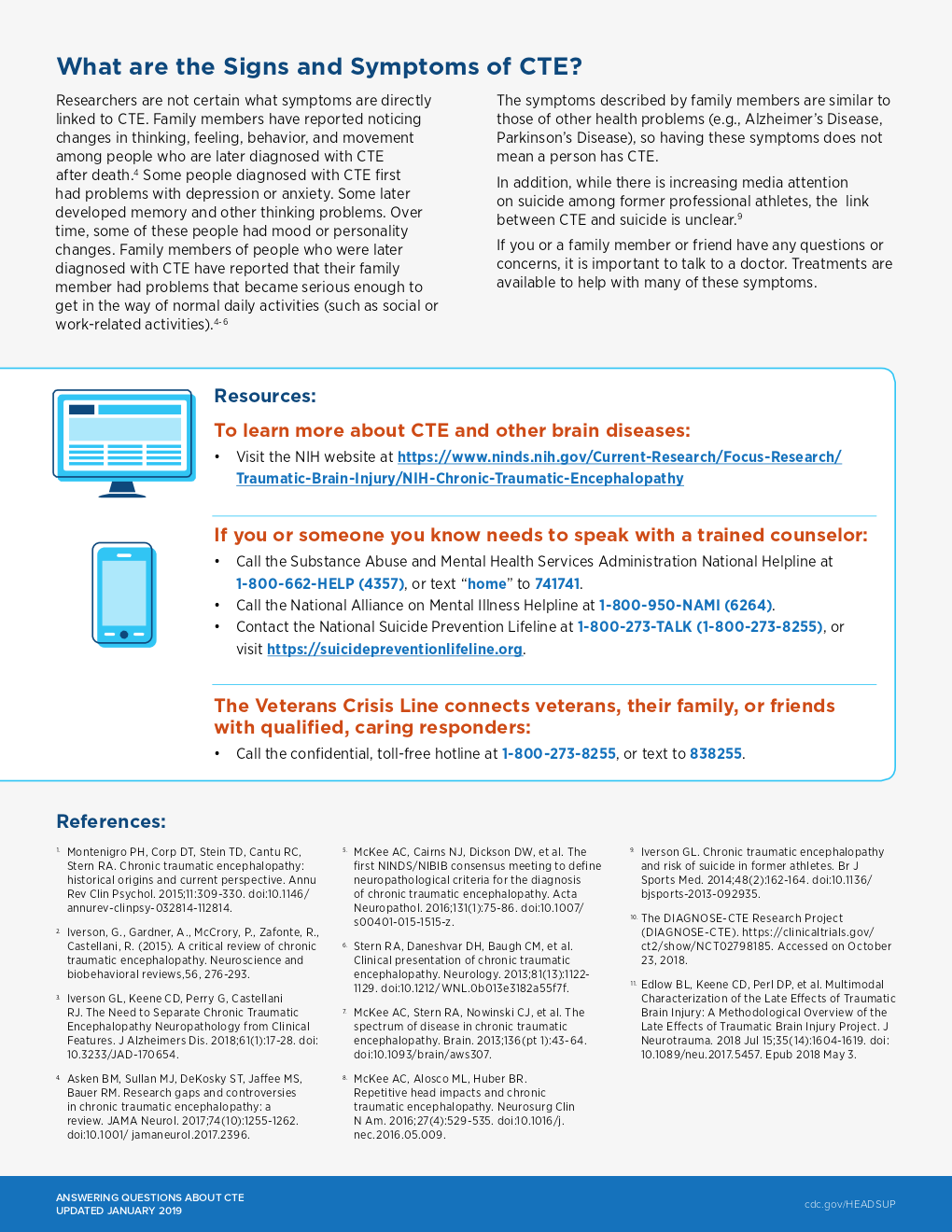
 MAHA CONCUSSION FACT SHEET
MAHA CONCUSSION FACT SHEET
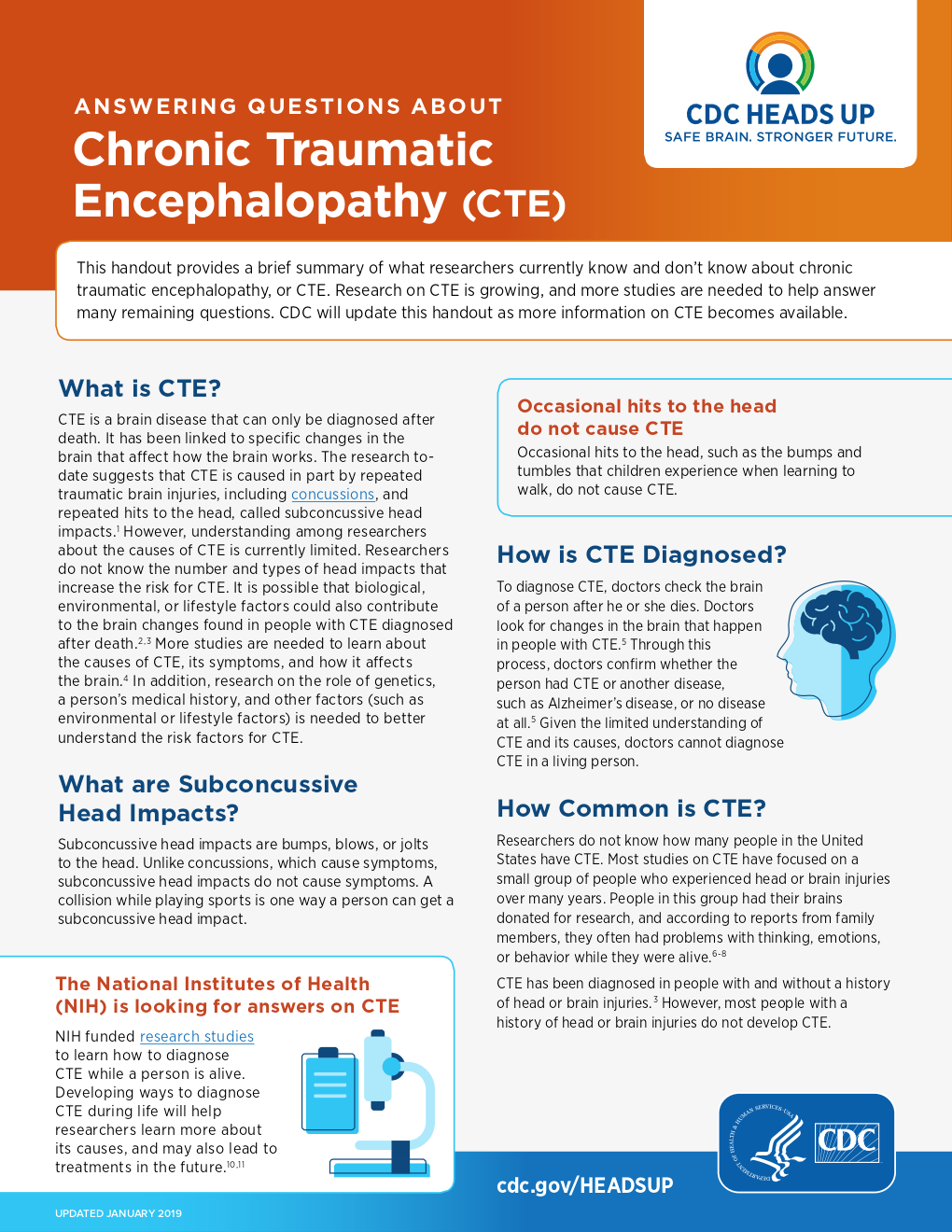
WHAT IS A CONCUSSION?
A concussion is a type of traumatic brain injury—or TBI—caused by a bump, blow, or jolt to the head or by a hit to the body that causes the head and brain to move quickly back and forth. This fast movement can cause the brain to bounce around or twist in the skull, creating chemical changes in the brain and sometimes stretching and damaging the brain cells.
HOW CAN I HELP KEEP MY CHILDREN SAFE?
Sports are a great way for children and teens to stay healthy and can help them do well in school. To help lower your children’s or teens’ chances of getting a concussion or other serious brain injury, you should:
- Help create a culture of safety for the team.
- Work with their coach to teach ways to lower the chances of getting a concussion.
- Talk with your children or teens about concussion and ask if they have concerns about reporting a concussion. Talk with them about their concerns; emphasize the importance of reporting concussions and taking time to recover from one.
- Ensure that they follow their coach’s rules for safety and the rules of the sport.
- Tell your children or teens that you expect them to always practice good sportsmanship.
- When appropriate for the sport or activity, teach your children or teens that they must wear a helmet to lower the chances of the most serious types of brain or head injury. However, there is no “concussion-proof” helmet. So, even with a helmet, it is important for children and teens to avoid hits to the head.
HOW CAN I SPOT A POSSIBLE CONCUSSION?
Children and teens who show or report one or more of the signs and symptoms listed below—or simply say they just “don’t feel right” after a bump, blow, or jolt to the head or body—may have a concussion or other serious brain injury.
Signs Observed by Parents or Coaches
- Appears dazed or stunned.
- Forgets an instruction, is confused about an assignment or position, or is unsure of the game, score, or opponent.
- Moves clumsily.
- Answers questions slowly.
- Loses consciousness (even briefly).
- Shows mood, behavior, or personality changes.
- Cannot recall events prior to or after a hit or fall.
Symptoms Reported by Children and Teens
- Headache or “pressure” in head.
- Nausea or vomiting.
- Balance problems or dizziness, or double or blurry vision.
- Bothered by light or noise.
- Feeling sluggish, hazy, foggy, or groggy.
- Confusion, or concentration or memory problems.
- Just not “feeling right,” or “feeling down.”
Talk with your children and teens about concussion. Tell them to report their concussion symptoms to you and their coach right away. Some children and teens think concussions are not serious or worry that if they report a concussion they will lose their position on the team or look weak. Be sure to remind them that it is better to miss one game than the whole season.
Concussions affect each child and teen differently. While most children and teens with a concussion feel better within a couple of weeks, some will have symptoms for months or longer. Talk with your children’s or teens’ health care provider about if their concussion symptoms do not go away or if they get worse after they return to their regular activities.
WHAT ARE MORE SERIOUS DANGER SIGNS TO LOOK OUT FOR?
In rare cases, a dangerous collection of blood (hematoma) may form on the brain after a bump, blow, or jolt to the head or body and can squeeze the brain against the skull. Call 9-1-1 or take your child or teen to the emergency department right away if, after a bump, blow, or jolt to the head or body, he or she has one or more of these danger signs:
- One pupil is larger than the other.
- Drowsiness or inability to wake up.
- A headache that gets worse and does not go away.
- Slurred speech, weakness, numbness, or decreased coordination.
- Repeated vomiting or nausea, convulsions, or seizures (shaking or twitching).
- Unusual behavior, increased confusion, restlessness, or agitation.
- Loss of consciousness (passed out/knocked out). Even a brief loss of consciousness should be taken seriously.
Children and teens who continue to play while having concussion symptoms or who return to play too soon—while the brain is still healing— have a greater chance of getting another concussion. A repeat concussion that occurs while the brain is still healing from the first injury can be very serious and can affect a child or teen for a lifetime. It can even be fatal.
What Should I Do If My Child or Teen Has a Possible Concussion? As a parent, if you think your child or teen may have a concussion, you should:
- Remove your child or teen from playing.
- Keep your child or teen out of play the day of the injury. Your child or teen should be seen by a health care provider and only return to play with permission from a health care provider who is experienced in evaluating for concussion.
- Ask your child’s or teen’s health care provider for written instructions on helping your child or teen return to school. You can give the instructions to your child’s or teen’s school nurse and teacher(s) and return-to-play instructions to the coach and/or athletic trainer.
Do not try to judge the severity of the injury yourself. Only a health care provider should assess a child or teen for a concussion. Concussion signs and symptoms often show up soon after the injury. But you may not know how serious the concussion is at first, and some symptoms may not show up for hours or days. The brain needs time to heal after a concussion. A child’s or teen’s return to school and sports should be a gradual process that is carefully managed and monitored by a health care provider.
To learn more, go to www.cdc.gov/HEADSUP or usahockey.com/safety-concussion
All sports and free play are associated with the risk of a concussion, including playing, officiating, or participating in ice hockey. It is important that all participants and parents learn about concussion prevention, recognition, treatment and return to play. A concussed brain needs time to heal, and the person is much more likely to have another concussion if they return too soon. Repeat concussions are usually more severe and take longer to heal.